For years, people with obstructive sleep apnea (OSA) have faced an uncomfortable reality—sleeping with a CPAP machine. While continuous positive airway pressure therapy remains the gold standard, not everyone can tolerate the bulk, the hose, the mask, or even the noise. But there’s a new solution gaining traction that’s both innovative and minimally invasive: Hypoglossal Nerve Stimulation (HNS).
This game-changing technology is quietly transforming the lives of sleep apnea sufferers—particularly those who’ve tried and failed traditional treatments. If you’re among the millions struggling to breathe at night, here’s everything you need to know about HNS, how it works, and why it might be your next best step toward restful sleep.
What Is Obstructive Sleep Apnea—and Why Does It Matter?
Obstructive Sleep Apnea (OSA) is more than just snoring. It’s a chronic condition where your airway repeatedly collapses during sleep, causing pauses in breathing. These pauses can last anywhere from a few seconds to over a minute—and they can happen hundreds of times a night.
The result? Poor oxygen flow, fragmented sleep, and a wide range of symptoms, from daytime fatigue and headaches to mood swings and memory issues.
Common Symptoms of OSA:
-
Loud, chronic snoring
-
Choking or gasping during sleep
-
Morning headaches
-
Excessive daytime drowsiness
-
Poor concentration and memory
-
Irritability and depression
OSA isn’t just a nuisance—it’s a serious health concern. Untreated, it increases the risk of hypertension, heart disease, stroke, Type 2 diabetes, and even accidents caused by drowsy driving.
The CPAP Conundrum: Effective But Not for Everyone
CPAP machines work by delivering constant air pressure through a mask to keep your airway open. But despite its clinical effectiveness, CPAP therapy has one big problem: adherence.
In fact, studies show that nearly half of CPAP users stop using their machines within the first year. The reasons range from discomfort and noise to claustrophobia and inconvenience. And when patients stop using CPAP, their sleep apnea—and the associated health risks—return in full force.
So what happens when CPAP isn’t the answer?
That’s where Hypoglossal Nerve Stimulation comes in.
What Is Hypoglossal Nerve Stimulation (HNS)?
HNS is a newer, FDA-approved therapy designed specifically for people with moderate to severe OSA who can’t tolerate CPAP. The most well-known device on the market is Inspire, though others are emerging in clinical research and development.
How It Works:
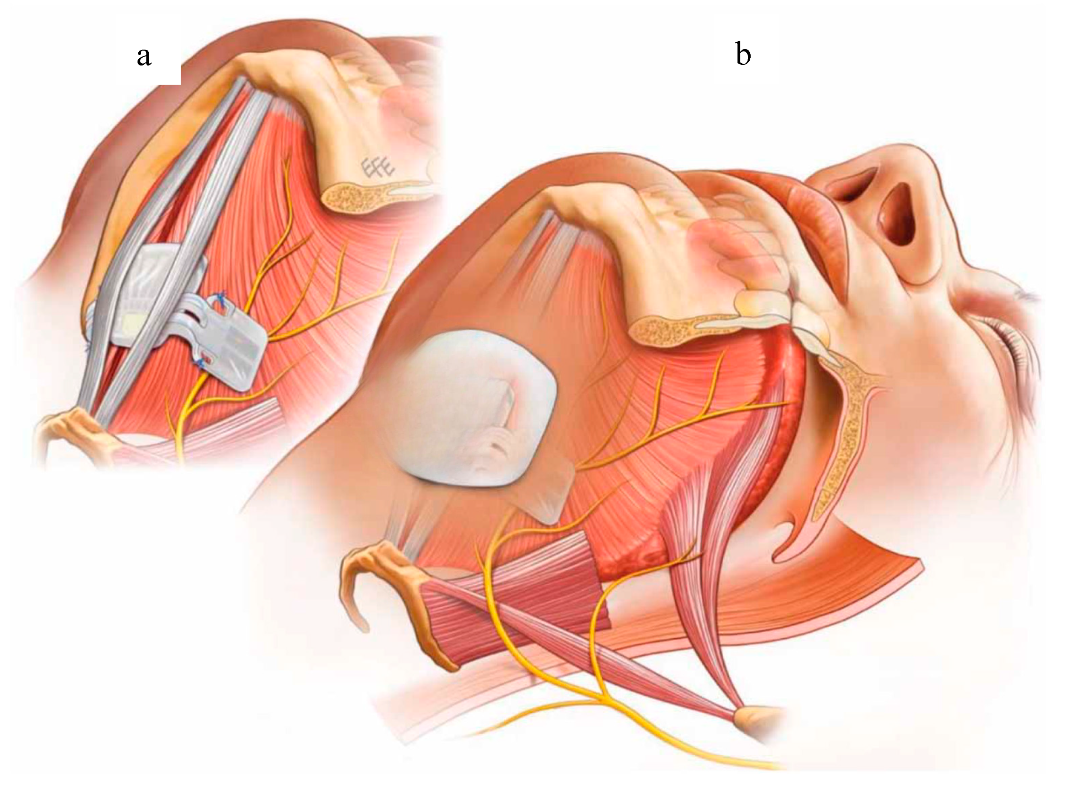
HNS involves implanting a small device—usually in an outpatient procedure—under the skin of the chest. This device sends gentle electrical pulses to the hypoglossal nerve, which controls the movement of the tongue.
Why the tongue? Because in many people with OSA, the tongue relaxes too much during sleep and falls back, blocking the airway. Stimulating the hypoglossal nerve helps keep the tongue forward and the airway open.
And the best part? The stimulation happens only when you’re sleeping. It’s synced with your breathing so you don’t feel it, and it doesn’t interfere with your day-to-day life.
Why HNS Is a Breakthrough
HNS isn’t just another device—it’s a targeted, personalized therapy that has been showing strong results across multiple clinical trials and real-world patient reports.
Key Benefits of HNS:
-
No mask or hose required
-
Customizable therapy based on your breathing patterns
-
Discreet and silent device
-
Minimal daily maintenance
-
High patient satisfaction and adherence rates
Patients often report improved sleep quality, reduced snoring, and better overall energy levels. And because it’s implantable, it removes many of the barriers that come with external devices.
Who Is a Good Candidate for Hypoglossal Nerve Stimulation?
Not everyone with OSA qualifies for HNS, and eligibility is carefully determined based on specific factors. Here’s what doctors typically look for:
Ideal HNS Candidates:
-
Moderate to severe obstructive sleep apnea (AHI between 15 and 65)
-
Inability to tolerate or benefit from CPAP therapy
-
Body Mass Index (BMI) of 32 or lower (though some exceptions are made)
-
No complete concentric collapse of the airway (confirmed through a sleep endoscopy)
Before proceeding with HNS, candidates usually undergo a drug-induced sleep endoscopy (DISE), which allows doctors to view the upper airway and determine if stimulation would be effective.
The Inspire Device: A Closer Look
Inspire is currently the leading HNS device on the market. Approved by the FDA in 2014, it has become increasingly popular as more insurance plans and providers recognize its effectiveness.
The Inspire System Includes:
-
A pulse generator implanted in the upper chest.
-
A breathing sensor lead that detects your breathing patterns.
-
A stimulation lead that sends signals to the hypoglossal nerve.
The device is turned on at night using a handheld remote. It automatically monitors and adjusts stimulation throughout the night to match your breathing.
What the Research Says
Multiple studies support the efficacy of HNS. The STAR trial, one of the largest Inspire studies to date, showed a 68% reduction in apnea-hypopnea index (AHI) and an 85% reduction in oxygen desaturation index (ODI) after one year. Patients also reported significant improvements in daytime sleepiness and quality of life.
Real-world data continues to reinforce these findings. According to a 2023 update from GlobeNewswire, HNS is gaining momentum across the U.S. and Europe as a reliable and minimally invasive treatment option. Inspire reports high patient satisfaction, with many users continuing therapy well beyond the one-year mark.
What to Expect: The HNS Procedure and Recovery
The procedure to implant the Inspire device is typically done under general anesthesia and takes about two hours. Most patients go home the same day.
Recovery Timeline:
-
Week 1–2: Mild swelling and soreness at the incision sites.
-
Week 3–4: Device check and follow-up visit with your sleep specialist.
-
Week 5–6: Activation of the device and customization of stimulation settings.
-
Month 2 onward: Regular sleep studies to monitor effectiveness and fine-tune therapy.
Most patients experience significant improvements in sleep within the first few months.
Living with HNS: What Patients Say
Patients often describe the experience as life-changing. Not having to wear a mask at night—or deal with air pressure noise—is a huge relief. The stimulation is gentle and usually undetectable while sleeping.
Common Experiences:
-
“I finally sleep through the night again.”
-
“My snoring is gone, and my partner is thrilled.”
-
“I feel energized during the day for the first time in years.”
-
“It’s easy to use—I just turn it on before bed.”
While not everyone responds equally, most patients report long-term satisfaction with their HNS device, especially compared to CPAP.
Insurance and Cost Considerations
One of the major concerns with HNS is cost—but insurance coverage is expanding. Inspire is covered by most major insurers, including Medicare, for eligible patients. The total cost can range between $30,000 and $40,000, including surgery and follow-ups, but many find it’s covered partially or fully by insurance.
It’s important to go through the pre-authorization process with your provider and sleep specialist to determine exact coverage and out-of-pocket expenses.
Are There Any Risks or Downsides?
As with any surgical procedure, there are risks involved. These may include infection, pain at the implant site, or nerve damage, though such complications are rare.
Other potential concerns include:
-
Limited availability of trained providers
-
Device not effective for certain types of airway collapse
-
Ongoing need for sleep monitoring and adjustments
That said, HNS is widely considered safe, and most complications are minor and manageable.
The Future of HNS and Sleep Apnea Treatment
HNS represents a powerful step forward in personalized sleep medicine. As research evolves, we may see even smaller devices, enhanced battery life, and expanded eligibility criteria—especially for people with higher BMIs or mixed forms of sleep apnea.
Companies like Inspire are also developing smart integration with sleep trackers and telehealth platforms to allow more dynamic therapy adjustments. With more people seeking non-invasive, non-mask solutions, HNS is well positioned to become a standard treatment option for a large group of patients.
Final Thoughts: Is HNS Right for You?
If you’ve been diagnosed with OSA and CPAP hasn’t worked for you, it’s time to talk to your sleep specialist about HNS. With high success rates, increasing insurance coverage, and minimal daily maintenance, it could be the solution that helps you reclaim your nights—and your days.
Quality sleep isn’t a luxury. It’s a necessity. And for many people, Hypoglossal Nerve Stimulation is making it possible.
FAQs About Hypoglossal Nerve Stimulation
1. Is HNS painful?
No, the stimulation is gentle and not painful. Most patients don’t feel it at all while sleeping.
2. How long does the device last?
The battery typically lasts 10–12 years. Replacement is done through a minor surgical procedure.
3. Can I have an MRI with an HNS device?
Some models are MRI-conditional. Always consult your doctor before undergoing an MRI.
4. Is HNS better than CPAP?
Not necessarily better—but ideal for those who can’t tolerate CPAP. It offers a highly effective alternative.
5. How soon will I see results?
Many patients notice improvements within weeks of activation, with continued optimization over time.
6. Can I travel with the Inspire device?
Yes! It’s fully portable. Just bring your remote and charger.
7. Will I need to replace the whole device?
Only the battery needs replacing after 10–12 years. The rest of the system usually stays intact.
8. Is there any risk of the device malfunctioning during sleep?
Rarely. The Inspire device is designed with safety mechanisms and remote-controlled shutoff.
9. How do I find out if I qualify for HNS?
Schedule an appointment with a certified Inspire-trained sleep specialist for evaluation and testing.